Antimicrobial resistance (AMR) is silently eroding the power of our antibiotics, posing one of the most significant threats to global health. It is not a disease itself, but a critical feature of many diseases.
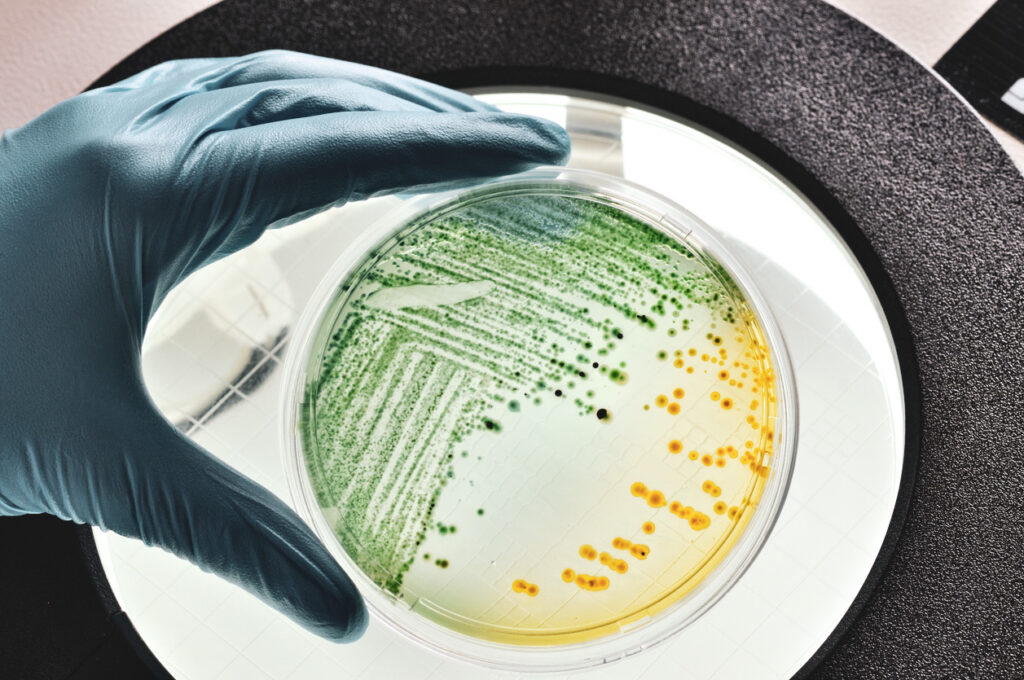
It occurs when microorganisms such as bacteria, viruses, fungi, and parasites evolve to resist the drugs designed to kill them, rendering treatments ineffective and infections harder to control.
Origins and escalation of AMR
AMR is a naturally occurring phenomenon where microbes evolve to withstand antimicrobial treatments. With a history stretching back more than 3.5 billion years, these microorganisms have continued to adapt and thrive throughout the Earth’s changing environments. This ancient resilience and drive to survive is resulting in microbes that are resistant to the drugs engineered specifically to kill them.
The overuse and misuse of antimicrobial medicines in humans and animals play a major role in accelerating AMR. In healthcare, the unnecessary prescription of antibiotics, combined with patients not completing their prescribed courses, contribute to resistance. In agriculture, the use of antibiotics for disease prevention has exacerbated the problem. Resistant bacteria also enter the environment through several ways including through wastewater and agricultural runoff, and there is an increasing body of evidence linking the warming climate with AMR. All combined, this leads to the exchange of resistant bacteria between people, animals, and the environment.
You have probably been impacted by antimicrobial resistance (AMR)
AMR isn’t just about untreatable infections that cause death; it’s already impacting everyday medical procedures and it’s likely already affected you personally. Patients often face treatment failures, leading to multiple rounds of antimicrobials as first, second, and even third-line treatments fail due to resistance.
For example, urinary tract infections, commonly caused by bacteria like Escherichia coli (e-coli), are increasingly difficult to treat as AMR limits the effectiveness of first-line antibiotics. This results in treatment failures, recurrent infections, and the need for broader-spectrum antibiotics that have more side effects and are often more expensive. Consequently, healthcare costs rise, illnesses are prolonged, and the risk of spreading resistant organisms increases.
If current trends continue, the consequences of AMR could be devastating.
Future forecasts indicate AMR deaths will rise steadily in the coming decades, increasing by almost 70% by 2050 compared to 2022, with older people being more greatly impacted.
It is estimated that by 2050, 39 million people will die from AMR infections.Economically, AMR could reduce global GDP by up to 5%, pushing millions into extreme poverty. The impact on healthcare systems would be severe, with routine surgeries and minor infections becoming high-risk due to the threat of untreatable infections.
In Australia, it is hard to quantify the exact number of deaths from AMR, partly because cause of death is often categorised under a patient’s primary condition. A 2022 report by CSIRO and AAMRNet suggested there are potentially as many as 5,276 deaths from AMR each year in Australia, while also highlighting the need for more accurate methods to understand the severity of the problem.
Addressing AMR also requires tackling the health and healthcare inequities that exist between urban areas and rural and remote regions, where the burden of AMR is higher. These disparities mean that not everyone has equal access to healthcare services, which can exacerbate the spread and impact of resistant infections. Rural and remote areas often face challenges with workforce, facilities, and diagnostic services, which can further delay the identification and appropriate treatment of resistant infections.
Preventing and controlling antimicrobial resistance (AMR)
While developing new antibiotics is an important aspect of the broader strategy, it should not be seen as a cure-all solution. Despite significant investment, this approach has yielded limited success. This highlights the importance of prioritising prevention.
Key strategies include:
- Improving antibiotic stewardship
This involves optimising the use of antibiotics in humans and animals to minimise the emergence of resistance. Healthcare providers must ensure antibiotics are prescribed only when necessary and that patients complete their full treatment courses.
- Enhancing infection prevention and control
Implementing stringent hygiene and infection-control measures in healthcare settings can reduce the spread of resistant infections. This includes hand hygiene, the use of personal protective equipment, and environmental cleaning. Following the National Hand Hygiene Initiative, Australia has demonstrated success in reducing drug-resistant infections in hospitals and maintains a high compliance rate.
- Research and Development
Investment into research and development for new vaccines, therapeutics and novel medical devices is essential. Vaccines play a crucial role in preventing infections that might otherwise require antibiotics, thereby slowing the development of resistance. For example, the influenza vaccine can help prevent secondary bacterial infections that often need antibiotic treatment.
- Raising public awareness
Educating the public on the dangers of antibiotic misuse and the importance of adhering to prescribed treatments is vital. Public health campaigns can also help reduce the demand for unnecessary antibiotics and reduce the expectation of patients to be prescribed antibiotics by their GP.
- One Health approach
Recognising the interconnectedness of human, animal, and environmental health, addressing AMR requires coordinated efforts and a one-health approach. This involves collaborative efforts across multiple sectors including health, agriculture and the environment to understand how AMR moves across all sectors and where intervention strategies can be best applied for maximum impact.
While AMR poses a daunting challenge, concerted efforts across multiple sectors can significantly curb its threat.
Prevention through responsible antimicrobial use, robust infection control, research, vaccination, and a One Health approach are key pillars in the fight against AMR, ensuring a healthier future for all.
Asaesja Young is an expert in translating complex scientific research into accessible information for the public, with a background in health and science communication, as well as significant experience in government and policy roles.



