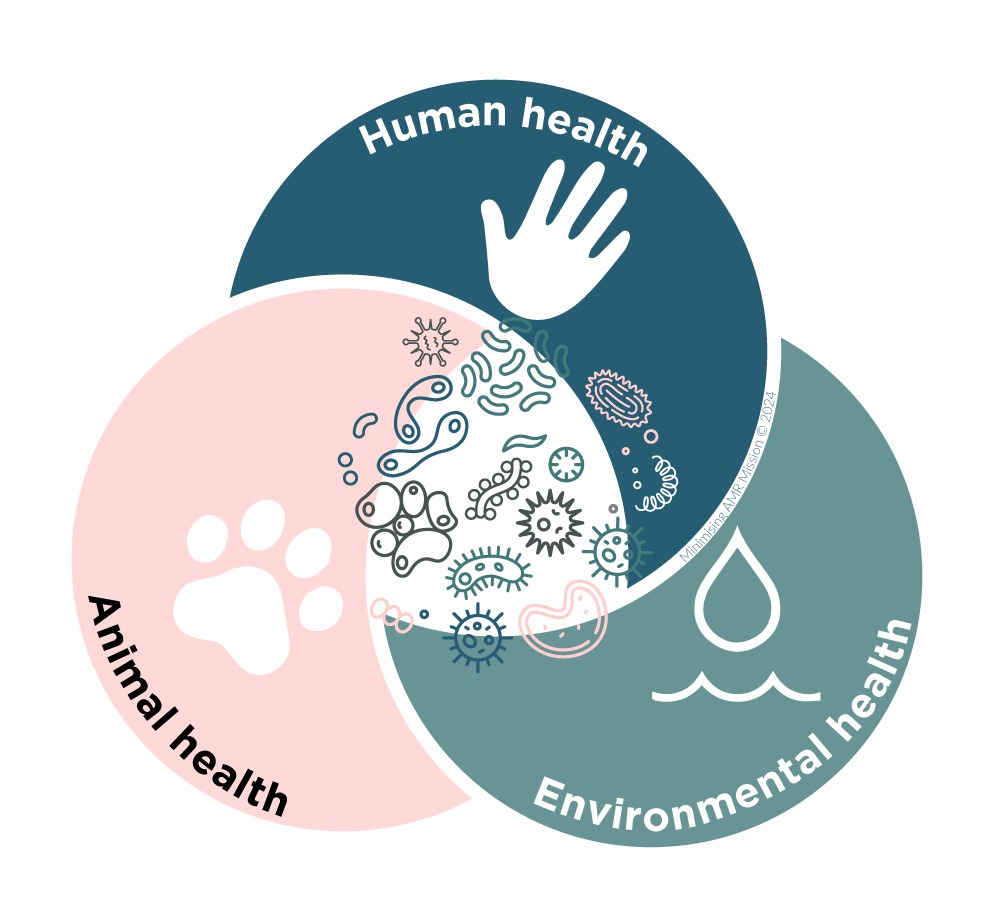
The role of One Health in addressing AMR
A One Health approach is based on the understanding that the health of people, animals, and ecosystems are interlinked and codependent. It promotes a collaborative, multi-sectoral, and transdisciplinary approach, working at local, regional, national, and global levels, while ensuring that solving a problem in one sector, does not inadvertently cause a problem for another.
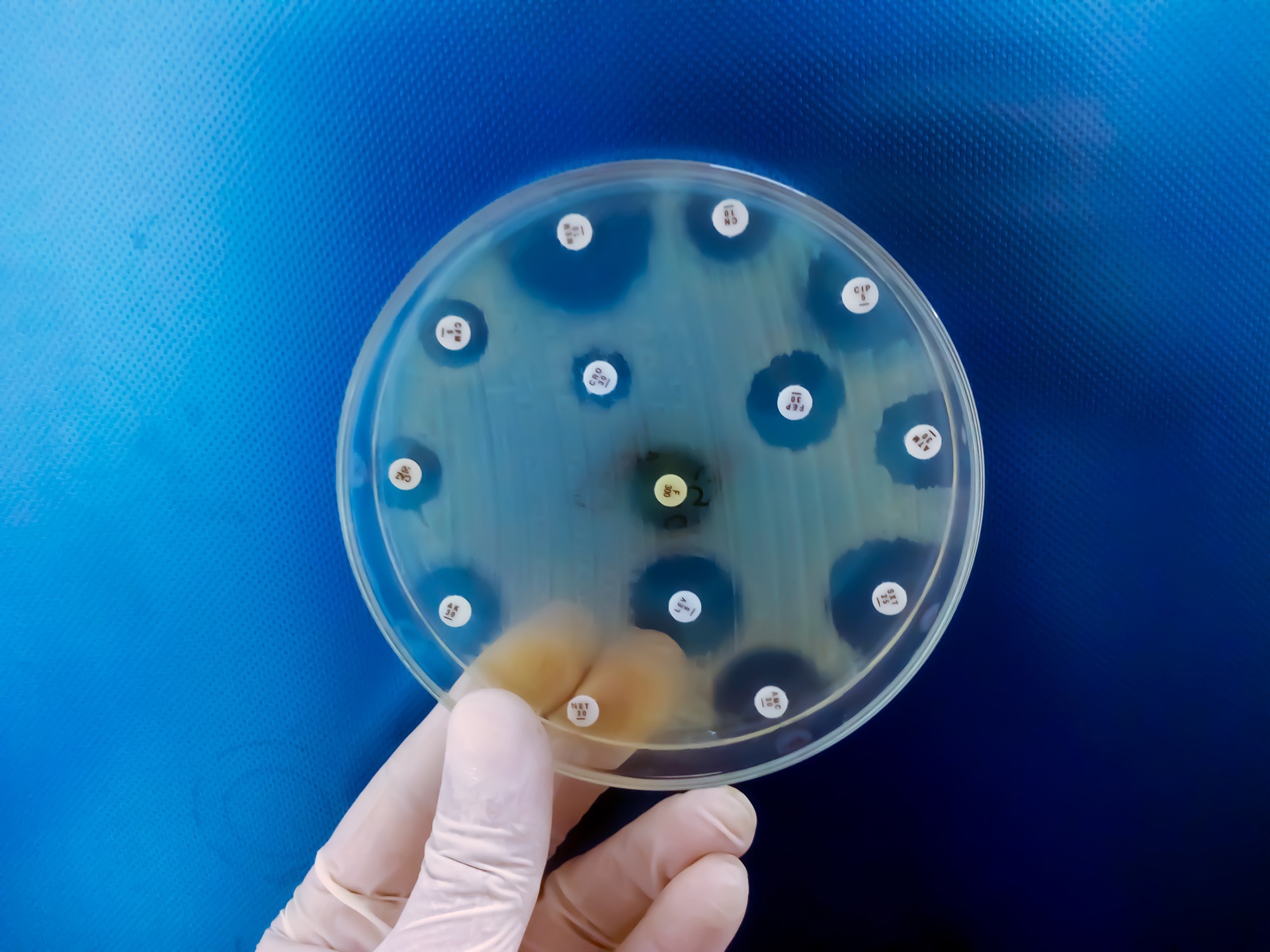
Antimicrobial resistance (AMR) is a global health threat that requires a One Health approach. AMR which arises when microorganisms evolve to resist the effects of antimicrobial drugs, making infections harder to treat and increasing the risk of disease spread, severe illness, and death.
In 2019, almost 5 million deaths were linked to AMR. By 2050 this could rise to 10 million each year, costing the global economy US$100 trillion. In Australia, deaths caused by AMR are believed to be significantly underreported, with recent research suggesting as many as 5,276 Australians are dying each year from untreatable infections.
Human health
In the context of AMR, the One Health approach involves coordinated efforts to reduce the misuse and overuse of antimicrobials in humans. This includes robust surveillance systems to monitor antimicrobial use and resistance patterns, promoting rational antibiotic use through stewardship programs, and enhancing infection prevention and control measures in healthcare settings.
Public education campaigns are critical to inform individuals about the risks of AMR and the importance of adhering to prescribed treatments. In Australia, the AURA surveillance system provides data and trends on antimicrobial use and resistance in people.
Animal health
The use of antibiotics in livestock for growth promotion and disease prevention has been essential for maintaining animal health and productivity. A One Health approach advocates for responsible antimicrobial use in animals, guided by veterinary oversight and regulations to ensure judicious use of critical antibiotics.
Strengthening veterinary services, improving animal husbandry practices, and promoting alternatives like vaccines and probiotics are key strategies. Australia has one of the world’s best records in minimising the use of antibiotics in food-producing animals.
Environmental health
The environment plays a crucial role in the transmission of resistant pathogens, with a growing body of evidence linking global warming with an increase in AMR.
Antibiotics and resistant bacteria can enter the environment through various routes, including agricultural runoff, wastewater, and the improper disposal of pharmaceutical waste.
The One Health approach emphasises the need for environmental monitoring and management practices to mitigate the spread of AMR. This includes improving wastewater-treatment processes, regulating the disposal of pharmaceutical waste, and reducing environmental contamination from agricultural sources.
Harnessing interdisciplinary collaboration
A key strength of the One Health approach is its emphasis on interdisciplinary collaboration across sectors, including public health, veterinary medicine, agriculture, environmental science, and social sciences. This collaborative framework facilitates the sharing of data and resources, enabling more effective surveillance, research, and policy making.
Effective surveillance and sensing systems are crucial for tracking the emergence and spread of AMR. One Health initiatives advocate for harmonised surveillance protocols and interoperable data across human, animal, and environmental health sectors, to provide a comprehensive understanding of AMR patterns and trends.
This integrated approach is key to combat AMR, and would empower a shift to preventative intervention strategies and evaluation. Despite the urgent need recognised across sectors and governments, Australia lacks a unified surveillance system.
Interdisciplinary research is essential for developing new strategies to combat AMR. The One Health approach promotes collaborative research to understand resistance mechanisms, develop new antimicrobial agents, and explore alternative treatments. Innovations in point-of-care diagnostic tools, vaccines, and infection-control technologies are critical to reducing antibiotic reliance.
Policies that promote responsible antimicrobial use across sectors are central to the One Health approach. This includes establishing regulatory frameworks to minimise the use of critical antimicrobials and incentivising the development of new vaccines, therapeutics, and devices. Policy and regulatory support help prevent AMR through the smarter design of farms, hospitals and other high-risk settings.
Challenges in implementing a One Health approach in Australia
Australia’s National Antimicrobial Resistance Strategy – 2020 and Beyond, produced by the Australian Government, set key actions, including: regulating the use of certain antibiotics in animal production; setting benchmarks for antimicrobial practices among healthcare providers; and, implementing antimicrobial stewardship programs. Despite this, Australia continues to have one of the highest antibiotic prescribing rates among developed nations. Furthermore, the lack of an integrated surveillance system hampers the ability to fully understand the extent of AMR and identify effective interventions.
A recent report by CSIRO and ATSE made two key recommendations to progress AMR management in Australia. The first called for a national and centralised coordination to: provide leadership; drive progress; ensure the implementation and evaluation of AMR interventions; integrate AMR management into urban and environmental planning; and, lead communication and engagement campaigns.
Their second recommendation was to better support the commercialisation process in Australia to help new AMR prevention and mitigation technologies enter the market.
Effective and long-lasting solutions for AMR require a comprehensive One Health approach, with coordinated action across all impacted sectors to safeguard the health of humans, animals, and the environment.