Inappropriate antibiotic use in human health significantly contributes to the global threat of antimicrobial resistance (AMR), with Australians being notable contributors. Better diagnostics have a vital role to play.
Reducing inappropriate antibiotic use goes hand in hand with reducing the chances of bacteria developing resistance, extending the usefulness of existing treatments and buying valuable time to research alternatives.
The key lies in finding better ways to identify a bug and then the best treatment. Currently, about 25% of antibiotics prescriptions in hospital settings are not appropriate for use: they’re either targeting more kinds of bacteria than they need to, eliminating good bacteria as well as bad, given to patients before surgery unnecessarily, or prescribed to patients who don’t need them.
In Australia, the standard way to identify what’s causing infection and the best treatment is to take a sample from a patient, grow the bug in culture in a laboratory, and then expose it to different antibiotics.
It’s effective, but it’s often just not fast enough. The turnaround time between taking a sample and getting results can be two to three days.
Dean Whiting, CEO at Pathology Technology Australia, says the risks of waiting before prescribing treatment are high.
“In two to three days, a patient can go from being stable to being in sepsis and close to death,” he says. “That’s two or three days you don’t have time for, which is why antibiotics are given straight away.”
Doctors may prescribe antibiotics to a sick patient immediately to prevent infections spiralling out of control, even before they know what infection they’re dealing with. That, in turn, drives the rise of AMR.

Is point-of-care testing the answer?
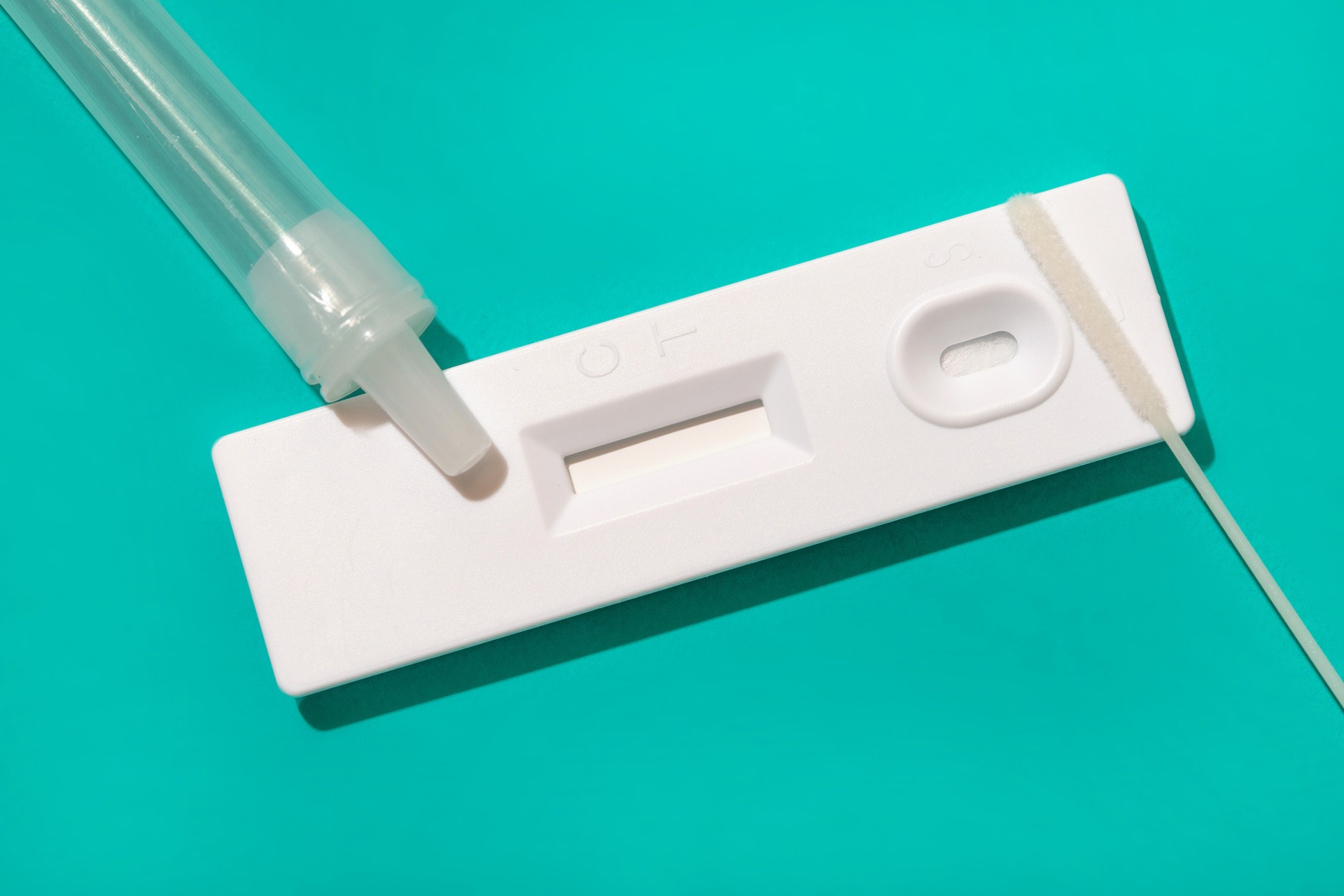
Point-of-care testing (PoCT) could play a vital role in reducing the inappropriate prescription of antibiotics. These diagnostic technologies enable medical practitioners to take samples and diagnose conditions on the spot, often while the patient is present. PoCT devices are commonly used to diagnose conditions like heart disease, diabetes, sepsis and COVID-19.
Several PoCT options to diagnose bacterial infections have been demonstrated internationally. “These tests can happen in a doctor’s surgery and within a few moments, a doctor can get a reliable indication about whether an infection can be treated with antibiotics,” says Mr Whiting.
C-reactive protein (CRP) testing examines the body’s inflammation response and within minutes can indicate if a respiratory infection is likely to be bacterial or viral. The reduced number of inappropriate antibiotic prescriptions has led to substantial cost savings in Sweden, Denmark, and Norway, where it is frequently used to detect respiratory tract infections in children and adults.
However, the use of CRP as a diagnostic on its own is somewhat controversial given gaps in scientific knowledge and the potential for significant variation in baseline levels due to time of sampling, age, pre-existing conditions and other medications.
FebriDx is an Australian invention, partly based on CRP testing, that analyses a blood sample from a finger prick. “It doesn’t rely on identifying the specific bacteria or the virus, but it uses biomarkers in blood and an algorithm to say if an infection is likely to be of bacterial or viral origin,” Mr Whiting says.
Rapid Antigen Tests (RATs) are available to indicate the presence of Strep A for example, which can be treated with targeted antibiotics
Syndromic testing is an increasingly available option, Mr Whiting says. These combine multiple tests for similar bugs into one place: a patient with flu-like symptoms, for example, might be tested for multiple influenza strains plus other common respiratory viruses in a single test.
These diagnostic tools are already used overseas, where they’ve proven to be clinically effective, and very quick to perform, resulting in substantial cost savings, and reduced inappropriate antibiotic prescribing.
“
Point-of-care testing can happen in a doctor’s surgery and within a few moments, a doctor can get a reliable indication about whether an infection can be treated with antibiotics.
Dean Whiting
Funding better diagnostic methods in Australia
The biggest barrier to increasing PoCT uptake in Australian general practice is funding. Most pathology testing performed in hospitals and commercial pathology labs is taxpayer funded. Some PoCT is funded through State and Territory health budgets, but very few are funded by Medicare.
Mr Whiting says it can be “devilishly difficult” to conduct accurate cost-benefit analyses of different testing methods.
“If the lab can do it for a few dollars, at high volume, while the point-of-care tests are more expensive , and you’re doing a handful of tests a day, of course the lab looks like a more economical option,” Mr Whiting says.
“But in the process of sending a patient away with a pathology form, getting the sample collected, sending that sample to a lab, getting the results back to the doctor, and then getting the patient back for a follow up appointment – in the context of a suspected infection, there are so many places where that process can fall down, which aren’t reflected in the value proposition of point-of-care testing.” He also notes that even when there are measurable benefits of a testing programme it often comes to an end when the grant funding ends,
This is where PoCT in community pharmacy settings could play an important role. An Australian feasibility study found more than 50% of participants “had their perceptions changed regarding their need for antibiotics”, according to a report by the Deeble Institute for Health Policy Research.
The report called for greater funding from the Australian Federal Government for PoCT in general practice and pharmacy settings. Mr Whiting agrees: “Hopefully we can have some very different conversations around point-of-care testing in the future.”
Emma Berthold has over a decade of experience across a variety of marketing and communications roles spanning not-for-profits, universities, government departments, learned academies and online marketing agencies.