Some of the highest reported rates of Antimicrobial Resistance (AMR) in Australia are among remote Indigenous communities. This issue is complex, and there are underlying factors that exacerbate these rates.
Professor Asha Bowen is Head of the Department of Infectious Diseases at Perth Children’s Hospital and says that without addressing the social determinants of health, little progress can be made on AMR in these Aboriginal and Torres Strait Islander communities.
“
This is not a factor of being an Indigenous person, it’s a factor of systemic racism and the impact this has on health due to a lack of a healthy living environment and it should not be accepted.
One of the fundamentals is housing, whether it be people being unhoused or having a home that is low-quality and unsafe. Low-quality housing conditions can contribute to poor health, and poor health can result in households living in worse housing circumstances, including overcrowding.
While many of the health threats of poor housing are common across disadvantaged population groups, the impact of colonisation and the relationship of Aboriginal and Torres Strait Islander people to their land add to the importance of housing conditions as a determinant of health for Indigenous Australians.
The role of the National Antimicrobial Resistance Strategy
Prof Bowen says that the failure to include remote Indigenous communities in either the first or second National Antimicrobial Resistance Strategy, despite concerted advocacy to the contrary, has meant there is a big gap in Australia’s AMR strategy. In addition, the social determinants of health’s connection to AMR in these communities has been overlooked, including the importance of well-maintained and appropriate housing.
“It’s a massive oversight and it definitely needs to be fixed,” Prof Bowen says.
“
I think it’s a really important advocacy piece that housing and living conditions need to improve as part of addressing antimicrobial resistance.
“In remote First Nations communities there are very high rates of skin and soft-tissue infections where Staph aureus and Strep A are key drivers, and these are interacting with the social determinants of health and environmental conditions.
“We are seeing rates of skin sores among these communities that are the highest in the world. Housing in particular is a factor there because there’s inadequate maintenance to enable healthy living to occur.”
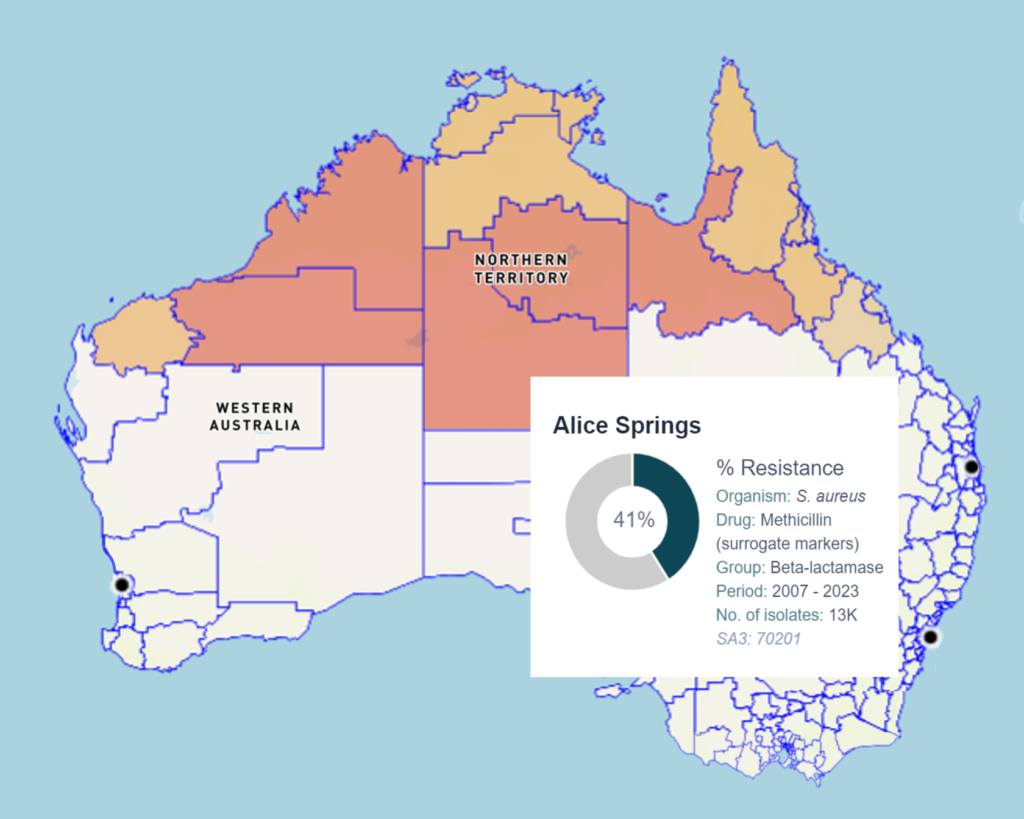
For example, in northern Australia the bacteria Staphylococcus aureus, (or S. aureus for short, also known as golden staph) causes skin and soft tissue infections. When S. aureus becomes resistant to the antibiotics commonly used to treat these infections, this is known as methicillin resistant S. aureus, or MRSA. The rates of MRSA in northern Australia are significantly higher than elsewhere in the country, with data showing infection rates in remote and very remote areas are double that of major cities.
As part of her PhD, Prof Bowen did a systematic review of the global rates of impetigo, a skin infection caused by bacteria that is often called ‘school sores’ because it is common among children. She found that in countries and regions that are considered impoverished, the prevalence of impetigo was between 7% and 10%, and in the Western Pacific it was around 29%. Yet in remote Aboriginal communities impetigo had a median prevalence of 45%.
Prof Bowen said that these skin and soft tissue infections often had the highly resistant MRSA as a pathogen, and when bloodstream infection rates were added, up to 60% of blood germ infections were connected to MRSA in the northern parts of Australia. This alters antibiotic choices, the success of treatment and increases mortality rates.
Mapping Australian AMR hotspots online
To map and respond to these high levels of AMR across northern Australia, an online platform called HOTspots has been developed. HOTspots is a disease surveillance and response program that monitors AMR infections in hospital and community clinic patients, and is hosted by CSIRO.
HOTspots launched in 2019 to support local clinicians to respond to the changing patterns of AMR within their region. Since then, it has grown into a program that provides education and training in collaboration with local stakeholders. Up-to-date surveillance data informs local treatment guidelines and clinical decision making.
“
Aboriginal and Torres Strait Islander cultures have survived on this land for millennia with deep resilience and stewardship and have so much to offer.
While HOTspots is currently focused on northern Australia, plans are in place to expand it to other geographic regions.
HOTspots show crossovers with social determinants of health outcomes
Running the HOTspots maps alongside where the social determinants of health are at their worst in Australia results in massive overlap.
Prof Bowen says addressing safe housing for both remote and urban-living Aboriginal and Torres Strait Islander people will improve health outcomes, alongside reducing AMR.
“This is not a factor of being an Indigenous person, it’s a factor of systemic racism and the impact this has on health due to a lack of a healthy living environment and it should not be accepted,” she says.
“I think it’s a really important advocacy piece that housing and living conditions need to improve as part of addressing antimicrobial resistance. We would solve many of these healthcare issues and not require antibiotics if we addressed housing, as it is all interconnected.
“Aboriginal and Torres Strait Islander cultures have survived on this land for millennia with deep resilience and stewardship and have so much to offer. There are many traditional remedies or bush medicines that can solve many of these problems and I think should be adjunct to what we offer from Western medicine for AMR and other health issues.”
Rebecca Thorpe is a journalist and communications specialist with decades of experience both in Australia and Europe.

